1. Definition PPH is the blood loss of 500ml or more (WHO, 2012)
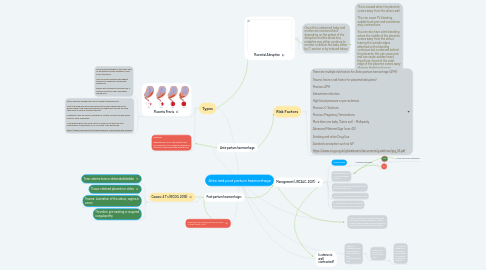
2. Types
2.1. Placenta Previa
2.1.1. The Placenta attaches to the lower part of the uterus and can partially or fully cover the cervix This can cause bleeding throughout pregnancy, especially during later pregnancy Babies will normally be delivered by C section due to the risk of bleeding during NVD
2.1.2. This is normally picked up at the 20-week ultrasound scan. Most low-lying placentas self rectify as the uterus grows and 9/10 women with a low-lying placenta will no longer have one by the time they come to deliver the baby (RCOG) Treatment relies on early recognition at routine scans and a plan being made as early as possible If the patient goes into early labour, a drug can be given to stop contractions to allow time for a C-section to be performed https://www.rcog.org.uk/en/patients/patient-leaflets/placenta-praevia/
2.2. Definition Bleeding from or in to the genital tract, occurring from 24+0 weeks of pregnancy and prior to the birth of the baby (RCOG
3. Ante partum haemorrhage
4. Post partum heamorrhage:
4.1. Causes: 4 T's (RCOG, 2016)
4.1.1. Tone: uterine tone or distended bladder
4.1.2. Tissue: retained placenta or clotts
4.1.3. Trauma: Laceration of the uterus, vagina or cervix
4.1.4. Thrombin: pre-existing or acquired coagulopathy
5. Check for perineal trauma. Apply external direct pressure with gauze/maternity pad.
5.1. Obtain 16G IV access and commence IV fluids
5.1.1. For ongoing bleeding IV tranexamic acid 1g over 10 minutes en route to hospital
6. SWAST Carbetocin. Given to those who are more than 20wks gestation, within 24hrs of delivery where haemorrhage has been uncontrolled by uterine massage
7. Is uterus is well contracted?
8. This is caused when the placenta comes away from the uterus wall. This can cause PV bleeding, sudden back pain and sometimes early contractions. You can also have silent bleeding where the middle of the placenta comes away from the uterus leaving the outside edges attached so the bleeding continues but is retained behind the placenta, this can cause pain and can cause sudden heavy blood loss if part of the outer edge of the placenta comes away allowing that blood loss to escape. This is generally only diagnosed by sudden onset back pain
9. Placental Abruption
9.1. Once this is detected, baby and mother are monitored and depending on the extent of the abruption and the blood loss, midwifes may either continue to monitor or deliver the baby either by C-section or by induced labour
10. Management (JRCALC, 2021)
10.1. Uterine atony
10.1.1. Placenta delivered?
10.1.1.1. Yes
10.1.1.1.1. firmly rub up a contraction
10.1.1.2. no
