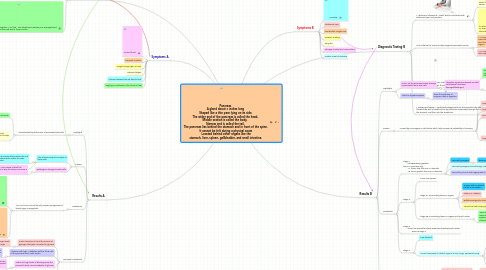
1. Symptoms A
1.1. Unusual thirst
1.2. Frequent urination
1.3. Weight change (gain or loss)
1.4. Extreme fatigue
1.5. Cuts and bruises that are slow to heal
1.6. Tingling or numbness in the hands or feet
2. Diagnostic Testing A
2.1. * Fasting blood sugar test. A blood sample will be taken after an overnight fast.
2.1.1. A fasting blood sugar level between 100 and 125 mg/dL (5.6 and 6.9 mmol/L) is considered prediabetes. If it's 126 mg/dL (7 mmol/L) or higher on two separate tests, you'll be diagnosed with diabetes.
2.2. * Random blood sugar test. A blood sample will be taken at a random time.
2.2.1. Regardless of when you last ate, a random blood sugar level of 200 milligrams per deciliter (mg/dL) — 11.1 millimoles per liter (mmol/L) — or higher suggests diabetes.
2.3. Lycated hemoglobin (A1C) test. This blood test indicates your average blood sugar level for the past two to three months.
2.3.1. It measures the percentage of blood sugar attached to hemoglobin, the oxygen-carrying protein in red blood cells.
2.3.1.1. The higher your blood sugar levels, the more hemoglobin you'll have with sugar attached. An A1C level of 6.5 percent or higher on two separate tests indicates that you have diabetes.
3. Results A
3.1. Highlights
3.1.1. characterized by destruction of pancreatic beta cells
3.1.1.1. -results in a deficiency of insulin
3.1.1.2. -results in overabundance of blood glucose since insulin isn’t present to stop its release
3.1.1.2.1. -interferes with filtration within the nephron
3.2. Causes
3.2.1. -the autoimmunity of one type of these cells
3.2.1.1. -ie the body attacks beta cells and renders them unable to make insulin
3.2.2. -pathogenic damage to Beta cells
3.2.2.1. Joining Idea – pure cause of what the pathogen was or why the body is immune is unknown
3.3. Treatments
3.3.1. -one can live a normal life with proper management of blood sugar management
3.3.1.1. -insulin medication
3.3.1.1.1. -effectively regulates amount of glycogen converted to glucose
3.3.1.2. -healthy diet and lifestyle
3.3.1.2.1. -limits the body’s needs for glucose and the excess amounts available in high quantities
3.4. Hormonal Mechanism
3.4.1. -insulin functions to limit the amount of glycogen that gets converted to glucose
3.4.1.1. -in effect keeping blood sugar levels low within an acceptable range
3.4.2. -however with type 1 diabetes mellitus the B cells of the pancreas don’t make insulin
3.4.2.1. -no insulin means no way of keeping glucose levels low -excess glucose can’t be converted to glycogen and stored
3.4.3. -with such high levels of blood glucose the proximal tubule cannot reabsorb all glucose
3.4.3.1. -excess glucose opposes the osmotic pressure of other actively transported solutes
3.4.3.1.1. -resultantly lots of water is lost in the kidney and this results in the symptoms of frequent urination and thirst
3.4.4. -the concentration of glucagon also increases
3.4.4.1. -this counteracts insulin and actually makes more glycogen into glucose and increases blood sugar levels even more, amplifying the effect
4. Symptoms B
4.1. Jaundice
4.2. Abdominal Pain.
4.3. Unintended Weight Loss
4.4. Nausea/Vomiting
4.5. Itchy skin
4.6. Changes in Stool and Urine Colour
4.7. Sudden onset of diabetes
5. Diagnostic Testing B
5.1. * Abdominal ultrasound: Useful test for individuals with abdominal pain and jaundice.
5.1.1. The test effectively detects gallstones which has symptoms similar to pancreatic cancer.
5.1.2. If a pancreatic tumor is seen on ultrasound, a CT scan is still necessary to obtain more information.
5.2. This is the test of choice to help diagnose pancreatic cancer.
5.2.1. A CT scan can accurately show whether the mass has extended beyond the pancreas and what the relation is to nearby blood vessels and organs
5.2.2. A CT scan can locate small tumours in the pancreas that might be missed by ultrasound.
5.2.2.1. - information vital to a surgeon planning an operation to remove the cancer.
5.3. * Percutaneous biopsy: This refers to a biopsy performed by inserting a needle through the skin into the body.
5.3.1. The procedure involves the insertion of a needle to the tumour by the guidance of ultrasound or CT scan.
5.3.1.1. Procedure done by a radiologist.
5.4. * Endoscopic biopsy: A gastroenterologist performs this procedure by inserting a flexible tube with a camera at the tip (called an endoscope) through the mouth, into the stomach, and then into the duodenum.
5.4.1. From here, a needle biopsy can be obtained with guidance from an ultrasound at the tip of the endoscope.
5.4.1.1. A person is heavily sedated for this procedure, and it is generally painless.
6. Results B
6.1. Highlights
6.1.1. -tumor on the pancreas causes damage to pancreatic tissue and cells
6.1.1.1. -therefore symptoms depend on what cells/tissues have been damaged/destroyed
6.1.1.1.1. -symptoms not evident until at more advanced due to similarity to gallstones for example
6.1.2. -lethal to digestive system
6.1.2.1. stops the synthesis of enzymes used in digestion
6.2. Causes
6.2.1. -caused by carcinogens or risk factors which help increase its probability of occuring
6.2.1.1. -smoking
6.2.1.2. -longstanding diabetes
6.2.1.3. -chronic pancreatitis
6.2.1.4. -hereditary conditions
6.2.1.4.1. -hereditary pancreatitis
6.2.1.4.2. -multiple endocrine neoplasia type 1 syndrome
6.2.1.4.3. -hereditary nonpolyposis colon cancer (HNPCC; Lynch syndrome)
6.2.1.4.4. -von Hippel-Lindau syndrome
6.2.1.4.5. -ataxia-telangiectasia
6.2.1.4.6. -familial atypical multiple mole melanoma syndrome (FAMMM).
6.3. Treatments
6.3.1. -Stage 1 -life expectancy greatest -tumor in pancreas only -1A, tumor less than 2cm in diameter -1B, tumor greater than 2cm in diameter
6.3.1.1. -removal by surgery
6.3.1.1.1. -best possible location and size
6.3.1.2. -removal by surgery, chemotherapy, radiation treatment
6.3.1.2.1. -size or location requires further intervention
6.3.1.3. -removal by clinical trial surgery with chemo and radiation
6.3.1.3.1. -when location and size give person not a great chance
6.3.2. -Stage 2
6.3.2.1. -tumor has spread
6.3.2.2. -stage 2A surrounding tissue or organs
6.3.2.2.1. -surgery with or without chemo and radiation
6.3.2.2.2. -chemo or radiation
6.3.2.2.3. -palliative surgery to unblock vessels and ducts (only addresses symptoms)
6.3.2.2.4. -clinical trial with varying amounts of chemo and radiation
6.3.2.3. -stage 2B, surrounding tissue or organs and lymph nodes
6.3.2.3.1. -same with more emphasis on more risky clinical trials involving experimental radiation or chemotherapy treatments
6.3.3. -Stage 3 -tumor has spread to blood vessels and nearby lymph nodes -same as stage 2
6.3.4. -Stage 4
6.3.4.1. -near terminal
6.3.4.2. -cancer has spread to distant organs, ie liver, lungs, peritoneal cavity
6.3.4.2.1. chemo
6.3.4.2.2. radiation
6.3.4.2.3. palliative treatments
6.3.4.2.4. no surgery
6.4. Hormonal Mechanisms
6.4.1. -blood sugar regulation
6.4.1.1. -insulin production compromised with damage to beta cells
6.4.1.1.1. -same effects as a lack of insulin with diabetes
6.4.1.2. -glucagon production compromised with damage to alpha cells
6.4.1.2.1. -glycogen therefore cannot be released from liver and turned to blood sugar without glucagon
6.4.2. -growth hormone
6.4.2.1. -somatostatin may not be made if Delta cells are damaged
6.4.2.1.1. -without this enzyme, maintenance of pancreatic cells is limited since no growth hormone is available to replace old cells with new ones
6.4.2.2. -delta cells may give somatostatin to all cancer cells to maximize their growth only
